BRCA1 and BRCA2 Genetic Testing
Using an individual’s genetic profile to customize his or her health care has become an integral part of my medical practice here in Austin, Texas. As medicine continues to focus on personalizing health care for each individual, I utilize a person’s genetic strengths and weaknesses to make decisions about how to better protect them against disease and how to optimally improve their health. With the recent focus on BRCA1 and BRCA2 genetic testing and the role of these genetic variations as a risk factor for breast and ovarian cancer, I have had many people ask me: Should I get tested? If I test positive, do I need to have a mastectomy? What are my risks and options if I do test positive? Here is what every woman should know.
What are BRCA Genes?
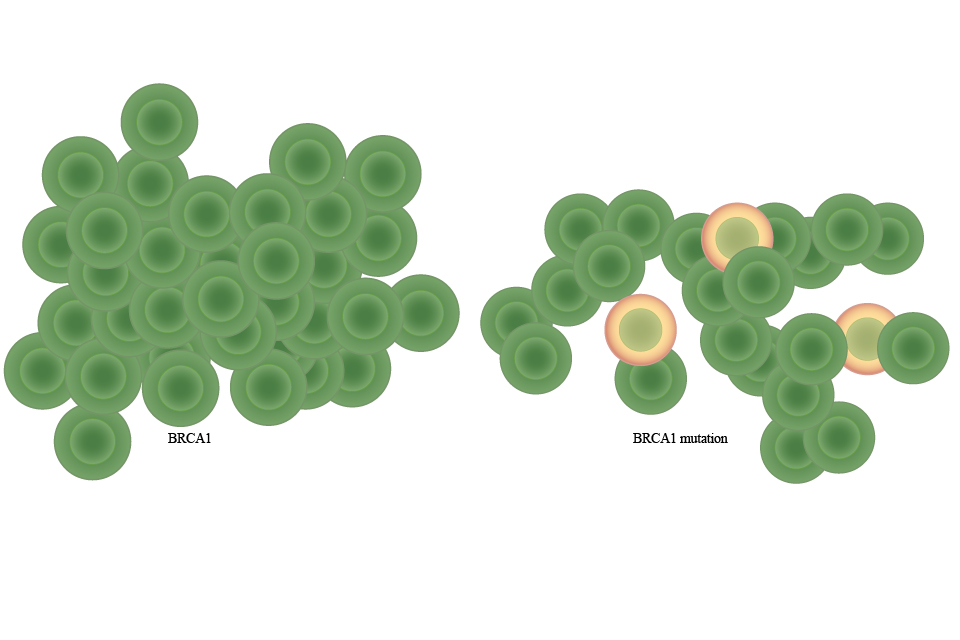
BRCA genes are tumor-suppressing genes that regulate cell growth and repair of damaged cells, preventing cells from becoming cancerous. Occasionally, alterations or mutations in these genes occur, preventing them from doing their job. This allows rapid cell growth in breast and ovarian cells and the inability of the body to repair damaged cells. When this occurs, it significantly increases the risk of breast and ovarian cancer.
What does getting tested consist of? And how do you know if you should get tested?
Getting tested requires taking a blood or saliva sample and sending it to a lab that specializes in BRCA testing where the genes are separated from the DNA and analyzed.
Because the percentage of Americans who carry the mutated gene is so small, BRCA testing is not for everyone. About .2 percent of Americans carry the BRCA mutation and, of the women in the U.S. who have breast cancer, only 5 percent of them have a BRCA mutation. However, women who have a strong family history of breast and ovarian cancer are the ones who should seriously consider getting tested. It is advised that you consult a genetic counselor before you do the test to evaluate the value of testing, and, after the test, to discuss your options and alternatives.
If you have a mutated gene, does that mean you have cancer?
Having a mutated gene does not necessarily mean cancer will develop, but it definitely puts you at a higher risk than people without the BRCA mutation. If one tests positive for the mutation, there is a 60 to 80 percent lifetime chance of developing breast cancer. This is in comparison with women without the mutation whose lifetime risk of breast cancer is 12 percent. Similarly, women with the faulty BRCA gene have an increased risk of developing ovarian cancer, with the lifetime risk being 60 perecent rather than the 1.4 percent, which is the risk in the general population.
If your test comes back negative, does that mean you cannot get cancer?
If your test turns out negative, implying you don’t have the mutated BRCA gene, this does not mean you will not get cancer. This simply suggests that your chance of developing breast cancer or ovarian cancer is the same as that of the rest of the population. You should still take precautionary measures and watch for signs on a regular basis, with regular monthly breast exams and screenings as recommended by your physician.






