I Can’t Run Because I Have Bad Knees
by Shannon Mitchel MD, PT
I cringe when I hear a person say, “I can’t run because I have bad knees.” It pains me to even type it. The problem with their problem is that the most common causes for pain under the kneecap can easily be fixed with plain and simple rehabilitation. However, if left unattended, those small problems can lead to inactivity (whether due to pain or fear of pain), surgery, weight gain, and eventually, the dreaded joint replacement. With obesity in this country on a meteoric rise and inactivity being one of the main reasons for this rise, this topic should interest everyone. Simply put, if you don’t have knee pain yourself, you certainly know someone who does.For those suffering from pain under the kneecap, you are not alone. Studies show this sort of pain is the most common leg problem that affects physical activity. Without proper diagnosis and treatment, knee pain will eventually sideline as many as one in four people.Proper diagnosis and treatment is key to pain-free knees. Those who eventually show up at my office have often been told they have “bad knees” or arthritis or are “just getting old.” As a doctor who is also a runner, the most maddening reason I hear is when these sufferers of knee pain are dismissed with a “Well, it’s because you run” diagnosis. All of these (and many more less than helpful reasons) delay accurate diagnosis and treatment.Anatomy of a Knee
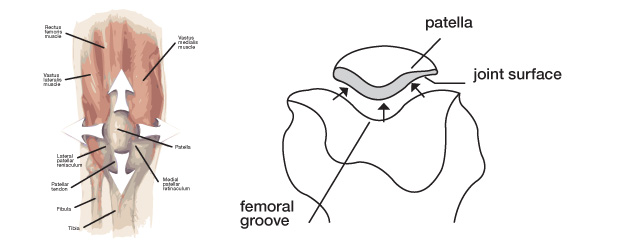
The knee joint is really made up of two joints. The one most people assume is their only joint is between the upper leg and lower leg. This is the hinge joint portion. The second, lesser-known joint lies between the kneecap and the thighbone. Ironically, it is this joint that causes most pain under the kneecap (and, from what I have seen in my patients, most knee pain across the board). The troublemaker, also known as the patellofemoral joint, is complicated from a physics standpoint because forces are pulling the joint in all directions (see image).
The kneecap is shaped more like a cone that slides up and down a groove formed in the knuckle portion of the thighbone rather than a flat disc (see Figure 2). When the forces that come from the muscles of the leg are out of balance and, as a result, pull in anything other than the 100 percent correct fashion, the bones bang into each other. If there is misalignment and the more pointed portion of the kneecap is not in the groove of the thighbone, this can over time damage the cartilage and lead to the pain we all hear about.
Since we all have heard how someone has “no cartilage left” in his or her knee, I wanted to explain what cartilage really is. Cartilage is the rather hard tissue that covers the ends of most bones in your body. If you have ever eaten a drumstick, visualize the white stuff on the knuckle portion of the bones. That’s cartilage. Because the blood supply to cartilage is not as efficient as to the muscles and other tissues in the body, damage will not heal as quickly. When someone with knee pain does not correct the underlying mechanical problem, the resulting damage will snowball. As the problem is misalignment and not overuse, inactivity or rest is never the answer. Of course, as with everything medical, the overall problem is always more complicated than this simple diagnosis, but for the sake of understanding, this is the best way to look at the problem most people have.
What Can Be Done?
The problem has been recognized; now, how is it fixed? A good medical doctor or physical therapist can, through a thorough history and physical, determine exactly what is causing discomfort in a particular case and prescribe the best course of rehab. As the exact cause and treatment is different in everyone, you cannot simply rely on the treatment your Uncle Frank used for his bum knee. Sometimes the pain can be due to weak hip muscles or weak leg muscles. More often, it is a combination of both. That is why it is extremely important to have guidance during rehabilitation so you can strengthen the muscles in the most efficient way possible with the least additional harm to the cartilage.
A good history and physical examination is the key. Generally, an MRI does not give additional information that is helpful. I realize many have been lead to believe it is the answer machine, but it is simply another piece of information that I rarely recommend unless rehab has failed or there has been some trauma to the knee. As for surgery, make this a last resort. Mark this in big red letters: Cartilage does not grow back. For every bit of cartilage you lose, the forces on the bones of your joint increase several times over, which can lead to early arthritis. An MRI may show frayed and damaged cartilage which, while not pretty to look at, is generally better than none at all in the long run.
Why Can’t a Surgeon Just Pull My Kneecap Where it Belongs?
If it were only that simple! As shown in Figure 1, the forces pulling the kneecap are generated mostly from various muscles and, as muscles stretch and get shorter, this simply does not work. Rehab is the key. One very large study in Europe looked at thousands of people with knee pain. In this study, the pain could be due to any reason at all. The results showed across all diagnoses that the stronger the leg muscles got, the less pain the person felt. Stronger muscles will lead to better joint mechanics and more activity which will in turn make the muscles even stronger, leading to less pain and a better lifestyle!
As with every medical problem, physicians should perform a thorough history and physical examination. This means they should actually touch patients’ knees. If your doctor does not, I suggest you find one who does!
Dr. Shannon Mitchel is a physician, physical therapist, and ultramarathon runner who practices occupational medicine at NOVA Medical Center in Austin. She also serves as medical director for various endurance events and maintains a small sports medicine private practice in South Austin.






